
Cancer arises when cells become uncontrolled while growing and dividing. This loss of control is due to genetic changes in the cells.
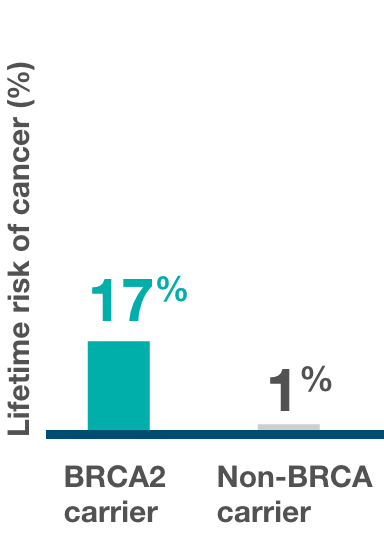
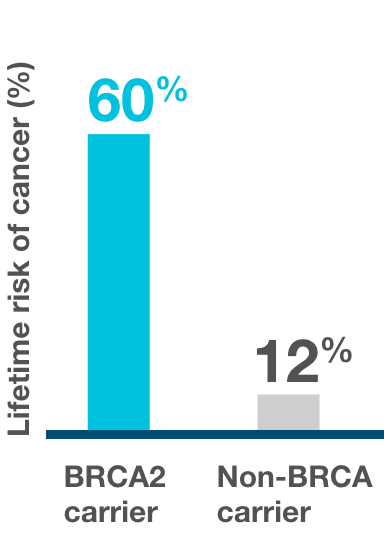
Hereditary breast and ovarian cancer syndrome (HBOC) refers to an inherited increased risk of breast, ovarian, and prostate cancer, and it is most commonly linked to an inherited genetic change, or in other words, a mutation in our BRCA genes. About 5-10% of breast cancers, 14-24% of ovarian cancers and 5-15% of prostate cancers are found to be hereditary. 1-5
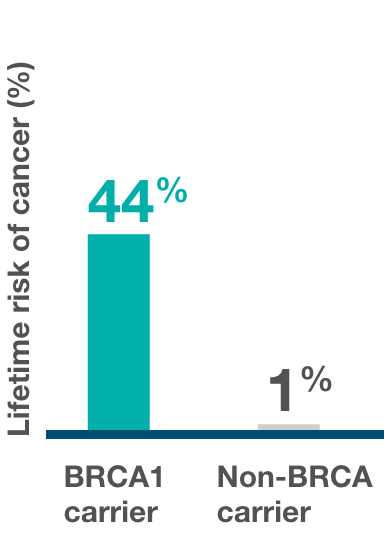
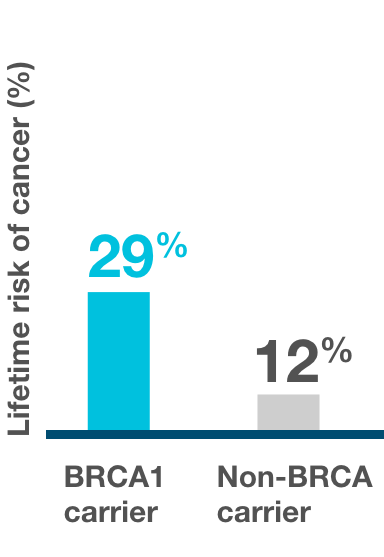
All of us have 2 sets of BRCA genes, BRCA1 and BRCA2. BRCA stands for BReast CAncer susceptibility gene. BRCA genes are “tumour suppressor genes”, which means that these genes have an important role to keep the cell in good condition. However, when these genes are mutated, they lose their ability to protect the cell, and this increases the risk of developing breast cancer, ovarian cancer, and prostate cancer.
Other cancers which may be caused by a faulty BRCA gene include fallopian tube cancer, peritoneal cancer, and pancreatic cancer.




This type of mutation is inherited from an individual’s parents.
They are often called hereditary mutations and can be inherited by the children.

This type of mutation is not inherited from an individual’s parents, but rather occurs randomly over their lifetime due to other risk factors. They are often called acquired mutations and cannot be inherited by the children.
If you have been diagnosed with breast, ovarian, or prostate cancer, you should consider BRCA mutation testing. Testing positive for a BRCA mutation could mean that you may be eligible for certain targeted therapies such as a PARP inhibitor.
In many countries, BRCA testing is routinely performed for patients newly diagnosed with breast, ovarian, and prostate cancer as recommended by guidelines. If your family has a history of cancer, speak to your doctor about getting a BRCA test.

International guidelines such as those from NCCN, SGO and ASCO recommend BRCA mutation testing for all epithelial non-mucinous ovarian cancer patients.10-13

It is recommended to test for BRCA mutation based on the following risk factors:14

If you have cancer, knowing your BRCA status can help you and your doctors decide on the best treatment option. It can also help inform others in your family about their cancer risk and allow them to take a proactive approach to manage their risk of developing cancer.
If you are a family member who does not have cancer, knowing your BRCA status will let you know if you are at an increased risk of developing certain cancers. From there, you and your doctor can screen for cancer more frequently or decide to take preventive action. Finding out that you have a BRCA mutation can also prompt other family members to get tested to see if they are at risk.
A blood or saliva sample is needed for testing hereditary BRCA mutations, while a tumour tissue is needed for testing somatic BRCA mutations. Tumour tissue is usually obtained from the surgery or biopsy performed if you have been diagnosed with cancer.
The sample taken is then sent to a laboratory that performs the tests. It usually takes 2-4 weeks to get the test results.

A tumour BRCA test can detect both germline and somatic mutations, however it does not differentiate between them. This type of test can be useful in deciding your treatment options.17

A blood or saliva BRCA test detects only germline BRCA mutations. Therefore, it is useful in informing whether you have an inherited BRCA mutation.18
Ideally, both tumour and germline BRCA testing should be performed and depending on the family history and therapeutic indications.
BRCA mutation testing can give several possible results:
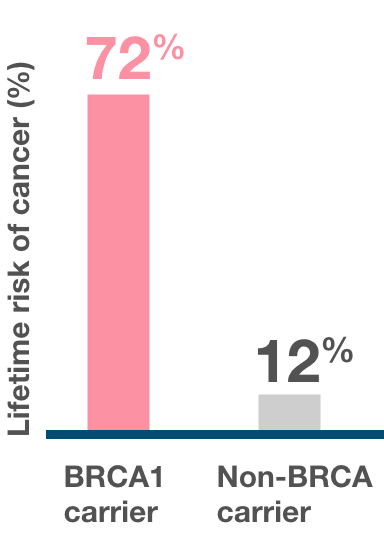
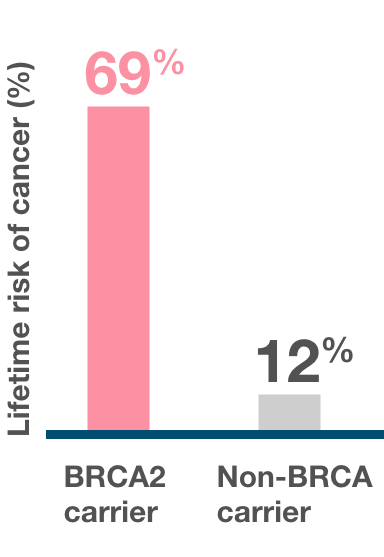
A positive test result indicates that a person has inherited a known harmful mutation in BRCA1 or BRCA2 and therefore has an increased risk of developing certain cancers.
However, a positive test result cannot confirm if and when an individual will develop cancer.
Knowing that you have a BRCA mutation can empower you to take action:
A negative test result means that the BRCA genes tested have no mutations.
An uncertain result means you have a BRCA genetic change but the impact of this change to the risk of cancer is unknown.
This is often referred to as a “genetic variant of unknown significance (VUS).” As more research is done, scientists will learn more about these genetic changes and the cancer risks associated with them.
If you have received this type of result, it is recommended that you contact a genetic counselor every 12 months to see if any additional information has been discovered which may lead to the reclassification of these results.